White Paper 2026-r01 — Full text
white paper
January 2026
Understanding Recurrent and Chronic Cystitis —
Psychological impact of an ongoing battle. Evidence from Italy.
Table of contents
Credits
European Cystitis Observatory (ECO)
Version V1
2026
DOI: 10.5281/zenodo.18185934
License: CC BY 4.0
How to cite (APA)
European Cystitis Observatory (ECO). (2026). Understanding Recurrent and Chronic Cystitis – Psychological impact of an ongoing battle.
Evidence from Italy.
(Versione V1). Zenodo. https://doi.org/10.5281/zenodo.18185934Doi 10 5281
How to cite (Harvard)
European Cystitis Observatory (ECO) (2026) «Understanding Recurrent and Chronic Cystitis – Psychological impact of an ongoing battle.
Evidence from Italy.».
Zenodo. doi:10.5281/zenodo.18185934.
Preface
Cystitis is still a persistent healthcare challenge for many women in Italy. Despite this, research exploring its impact on daily life—by analyzing the psychological, social, and economic factors that influence it—remains surprisingly limited.
With this white paper, Dimann launches the first in a series of studies aimed at gaining a deeper understanding of the social and behavioral dynamics surrounding cystitis, considering them both as possible causes and as consequences of the condition.
This first publication highlights two key aspects: on the one hand, the lack of data and research on the real impact of cystitis in everyday life; on the other, the tangible burden this condition places on women every single day.
Executive summary
In today’s data-driven world, cystitis still represents a blind spot. This white paper was created with the aim of presenting the Dimann dataset, which offers an unprecedented perspective on the daily challenges, risk factors, and psychological weight of cystitis on the lives of those affected.
Overview
Cystitis is a major public health issue, yet it is still often underestimated.
It primarily affects women, and its incidence increases significantly with age, becoming particularly common among older people. A substantial proportion of patients develop recurrent or chronic cystitis, which involves persistent pain, discomfort, and emotional distress, with a profound impact on quality of life and productivity.
Despite this, available data and research on the social and behavioral aspects of cystitis are very limited, revealing important gaps in the understanding of risk factors and the broader implications of cystitis.
In this context, the Dimann dataset introduces a valuable and innovative, person-centered perspective, and makes it possible to analyze the affected population with an unprecedented level of detail.
With over 34,000 questionnaires collected across Europe, the dataset represents the largest and most comprehensive snapshot ever created of people living with cystitis.
This resource makes it possible both to analyze behavioral risk factors and to assess consequences on quality of life—two dimensions often overlooked in traditional clinical research.
In particular, the data highlight the strong psychological burden of the condition, revealing its wide-ranging impact on everyday life, interpersonal relationships, and emotional health.
This new body of evidence reframes cystitis not only as a clinical issue, but also as a social one, underscoring the urgency of an integrated intervention that includes more effective diagnostic and therapeutic processes, targeted preventive actions, and comprehensive patient support.
Introduction
This section introduces cystitis and the challenges associated with it, outlining its causes, prevalence, different types of infection, and the most common symptoms.
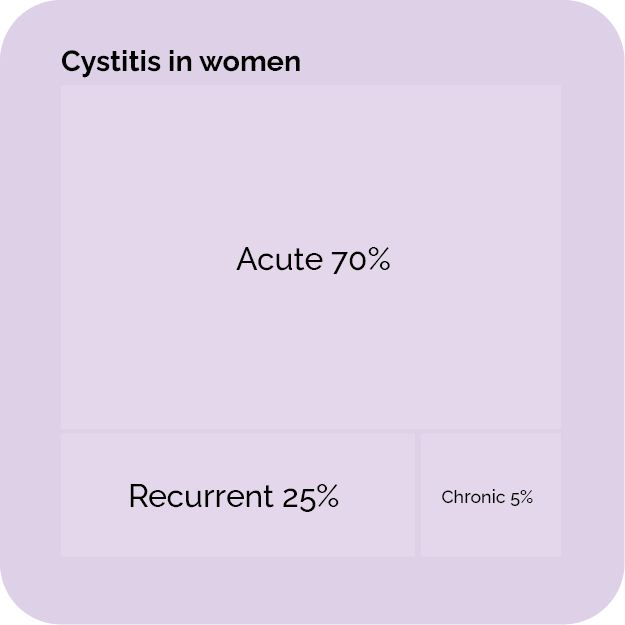
Cystitis is a urinary tract infection (UTI) that presents as inflammation of the bladder wall.. It is estimated to affect about 40–60% of women worldwide at least once in their lifetime.
Among them, over 20% experience recurrent episodes and at least 5% develop a chronic form that can persist for years [1-2].What appears to be an isolated infection often turns, in many cases, into a long-lasting and debilitating condition.
Women are significantly more at risk of developing cystitis than men, mainly due to an anatomical difference: the female urethra is much shorter (about 5 cm, compared to 16 cm in men), offering bacteria a more direct path to the bladder [3].
In addition to this structural vulnerability, hormonal factors play a role—particularly reduced estrogen levels, whether physiologically with age or linked to certain conditions—which can alter the balance of the vaginal and intestinal microbiota, creating a favorable environment for pathogenic bacteria to proliferate.
Sexual activity, pregnancy, and the use of certain contraceptive methods can also increase infection risk by modifying the internal balance or mechanically facilitating bacterial ascent.
For both sexes, certain unhealthy habits can increase the likelihood of developing an infection.. Among the most relevant factors are insufficient hydration, poor diet, smoking, disrupted sleep rhythms, chronic stress, and irregular urination habits.
Taken together, these elements show how cystitis does not stem from a single vulnerability, but rather results from multiple concomitant factors.
In men, although cystitis is less frequent, the risk increases significantly with age, often in association with benign prostatic hyperplasia or the presence of other conditions.
The incidence of chronic cystitis is likely underestimated, because periods of remission may lead to misclassifying some cases as recurrent forms.
Although only a minority of cases develop into severe complications, such as kidney failure or sepsis [4], the vast majority of patients live with a constellation of persistent and debilitating symptoms. . The most common include burning during urination, increased frequency and urgency, and pain localized in the lower abdomen [5].
These manifestations can be deeply disablinginterfering with daily activities. Moreover, what makes cystitis particularly difficult is its tendency to become recurrent—often resistant to conventional therapies and capable of reappearing cyclically. Over time, the impact goes well beyond physical discomfort: recurrent episodes generate uncertainty, anxiety, and a sense of vulnerability, and can lead to isolation or a perceived loss of autonomy [8]. . In this way, recurrent or chronic cystitis becomes far more than a simple medical condition: it becomes a long-term psychosocial burden capable of significantly reducing quality of life.
The recurrent nature of cystitis depends on specific predisposing factors and triggers.. The spectrum of infections is dominated by a relatively small group of pathogens: the most frequent isEscherichia coli, followed by Klebsiella pneumoniae, Proteus mirabilis, Enterococcus faecalis, Enterobacter cloacae, and Staphylococcus saprophyticus [9]. . Together, these microorganisms account for the majority of urinary infections, each with its own virulence factors and resistance mechanisms that influence disease course.
These pathogens are not merely “passive invaders”: they possess a complex set of virulence strategies enabling them to adhere firmly to the urothelial epithelium, evade the host immune defenses, and establish protected reservoirs within the urinary tract that can reactivate infection when conditions become favorable—even after completing therapy.
Such adaptability explains why many patients experience relapses even after apparent therapeutic success.
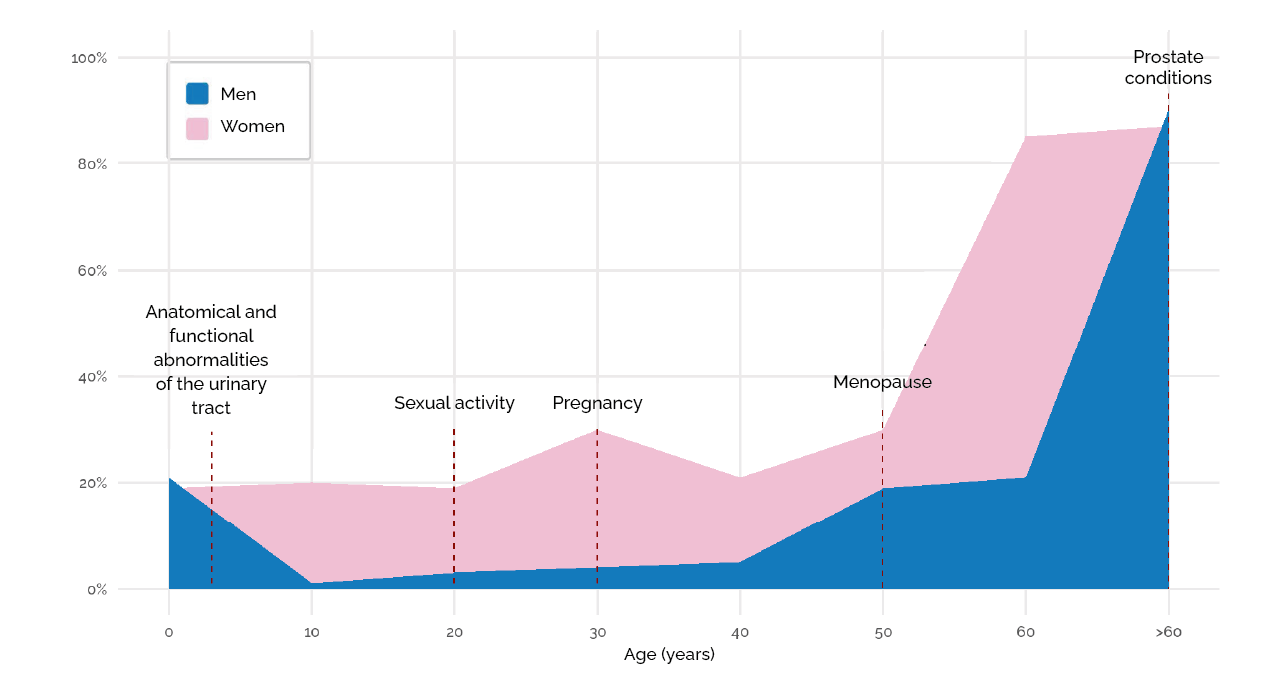
In women, prevalence increases in connection with sexual activity, pregnancy, and menopause; in men, risk grows mainly after age 60, in relation to prostatic conditions.
Adapted from: AOGOI. “Urinary tract infections in women from pre-adolescence to adulthood” [6].
Model by: Zamparini E., G. Ital. Nefrol. (2012) [7].
As a result, the relapse cycle becomes hard to break: each new episode increases patient discomfort and raises the risk of antibiotic resistance.
In some cases, the infection progresses beyond recurrence, taking on a chronic form that can persist over time without complete resolution. Chronic cystitis often develops due to incomplete or delayed treatments, missed diagnoses, or sometimes the absence of appropriate therapeutic intervention.. Unlike recurrent cystitis—where symptoms alternate with remission periods—the chronic form is characterized by continuous, uninterrupted discomfort.
Diagnosis and therapy also remain a major challenge. Urine culture, considered the only truly definitive diagnostic tool for urinary infections, is not performed regularly in everyday clinical practice; moreover, many patients, underestimating or misinterpreting symptoms, delay medical evaluation.
At the same time, healthcare providers sometimes resort to empiric antibiotic therapy [9],especially in cases where symptom relief is prioritized over diagnostic confirmation. While this approach may offer temporary improvement, it carries significant risks.
The absence of culture-supported diagnosis frequently leads to inappropriate antibiotic selection, incomplete pathogen eradication, and a higher likelihood of recurrence.. Even more concerning, widespread empiric therapy promotes antimicrobial resistance.
Previous studies [9] have shown that indiscriminate antibiotic prescribing not only reduces cure rates but also prolongs hospital stays, increases relapse risk, and accelerates the emergence of resistance. This triggers a vicious cycle in which treatments become progressively less effective, putting pressure on both patients and the healthcare system as a whole.
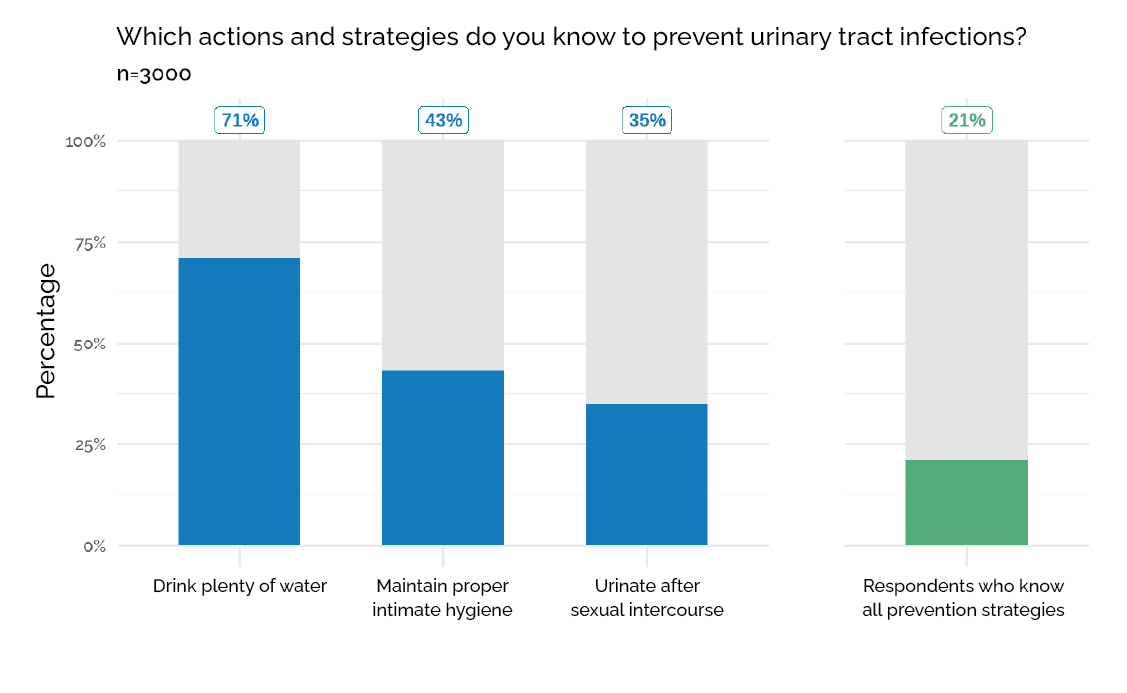
Over 3,000 citizens from Spain, France, Germany, the United Kingdom, and Italy were interviewed about their knowledge and experience regarding UTIs.
Only one in five people was able to identify all main prevention strategies.Dati: European Association of Urology (EAU), 22–26 september 2025 [14].
Data and perspectives in the Italian context
This section highlights the lack of cystitis data in Italy and presents the Dimann dataset as a valuable resource to deepen understanding of the causes and impact of this condition.
Within the Italian healthcare system, cystitis is one of the most common conditions.. Despite its prevalence, accurately estimating the true impact of cystitis in Italy remains complex—especially regarding causes, risk factors, epidemiological trends, and consequences on the lives of affected people. For instance, non-uniform diagnostic criteria and heterogeneous case definitions make it difficult to compare studies and clinical settings [10].. Additionally, many individuals experiencing mild or recurrent symptoms tend not to consult a physician, leading to underestimation in national surveillance systems and official statistics.
Data collection in Italy is further complicated by strong regional variability and fragmentation of health information systems, which hinder building a unified epidemiological picture [11]. . Moreover, while hospital registries and administrative databases mainly capture more severe or complicated UTIs, the vast majority of uncomplicated cystitis cases remain excluded from official statistics.
Recent studies have highlighted major gaps in the evidence available for the Italian context, emphasizing that data remain dispersed and inconsistent [10–12].
Furthermore, available epidemiological studies often group cystitis within broader UTI categories, thereby obscuring patterns specific to cystitis and its risk factors. Differences related to age, comorbidities, sexual behavior, and hormonal status further contribute to population heterogeneity, making extrapolation from limited samples unreliable.
Beyond the clinical dimension, the real impact of cystitis extends to quality of life and socioeconomic burden, causing reduced productivity, sexual distress, and psychological stress—factors rarely considered in existing research [12].
Overall, current evidence suggests that the estimated burden of cystitis in Italy underestimates its real impact on the population, both clinically and socioeconomically.
The Dimann dataset
In this context, the Dimann dataset represents a valuable opportunity to analyze a large sample of individuals affected by cystitis in Europe.
Collected as part of assessing D-mannose buyers in order to assign targeted products, the database includes over 34,000 questionnaires from four European countries, providing an extensive data foundation to address questions that have so far remained largely unexplored.
The data include, for example, behavioral factors associated with the onset of cystitis—such as personal hygiene, dietary habits, stress levels, and other psychological or lifestyle-related factors—all recognized for their potential to guide personalized prevention strategies and significantly reduce recurrence risk [13].
Beyond identifying risk factors, the dataset also highlights the profound impact of cystitis on everyday functioning and emotional wellbeing, showing to what extent recurring pain and uncertainty affect quality of life and offering a rare patient-centered perspective.
With over 30 items dedicated to sociodemographic characteristics, dietary habits, clinical management of cystitis, and its impact on daily life and activities, the dataset provides a comprehensive view of both behavioral risk factors and psychological consequences linked to the condition.
Currently, the dataset includes participants from Italy, France, Germany, and Spain, ensuring broad European representativeness, with further expansion planned in the coming months.
The Dimann dataset (Italian sample overview)
This section provides a preliminary overview of the sociodemographic composition of the Italian sample within the Dimann dataset, along with the main cystitis-related variables.
For Italian participants, the dataset includes over 25,000 observations collected between 2022 and 2025.
Each record contains responses to all sections of the questionnaire, allowing a full analysis of demographic characteristics, psychological and behavioral patterns, and reported symptoms.
Gender
In the Italian sample, a clear female predominance emerged, with 98.1% women compared to 1.7% men. This female predominance is likely linked to the targeting of Dimann products, which are primarily aimed at women. The remaining 0.2% selected the “other” category.
Age
Regarding age, individuals in the sample range from 18 to 99 years; however, participants over 60 are less represented than younger groups. The mean age is 40, with a median of 39, indicating a right-skewed distribution.. The third quartile (52 years) shows that 75% of respondents are 52 or younger. These values suggest the dataset mainly represents adults in the young and middle-age range.
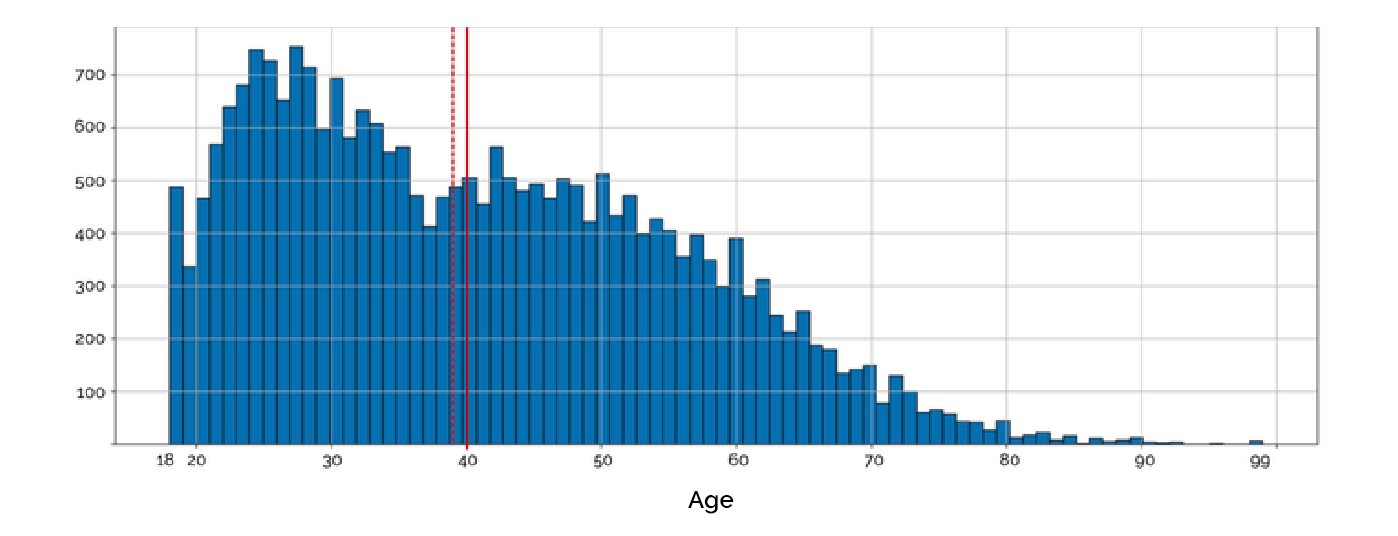
Participant ages range from 18 to 99. The majority are under 60, indicating a sample skewed toward young and middle-aged adults. In the histogram, the solid red line represents the mean age (40), while the dashed red line indicates the median age (39), both showing a concentration of responses in early and mid-adulthood.
The third quartile is 52 years, meaning 75% of respondents are 52 or younger (Table 1).
However, the distribution observed among younger participants closely reflects the model proposed by Zamparini [7], which describes cystitis frequency across different life stages.
As shown in the histogram, the number of respondents follows a pattern consistent with known epidemiological trends: higher incidence in young and middle adulthood, life periods typically associated with higher sexual activity, pregnancy, and then menopause.
Unlike Zamparini’s model, however, the histogram shows an opposite pattern beyond age 55.
This anomaly does not indicate a real decline in cystitis incidence, but may rather reflect sample characteristics: individuals over 55 are less represented, possibly due to a lower tendency to respond to questions or because they are less reached by the brand’s marketing tools.
The sharp variations after this age threshold therefore stem from participation bias rather than an actual epidemiological change.
Actions taken to investigate cystitis
Understanding how people approach cystitis investigation is a valuable resource to assess awareness and diagnostic behaviors. In the Dimann dataset, respondents report a variety of actions taken after symptom onset.
Responses include:
- Urine culture with antibiogram
- Laboratory urine tests
- Urine dipstick test
- Medical consultation (without diagnostic tests)
- No diagnostic action
Respondents appear to move along a broad spectrum of approaches, ranging from self-management and informal testing to medical consultation, each reflecting different levels of access to care and engagement with healthcare services.
The marked variability observed in the distribution of responses (Figure 5) reflects the fragmentation and inconsistency of diagnostic pathways experienced by many respondents.
This is shown by the fact that, although the majority (about 70%) report having had either a urine culture with antibiogram (55%) or laboratory urine tests (15%), an additional 19% state they performed no diagnostic tests beyond completing the questionnaire itself.
This wide discrepancy highlights the coexistence of proactive and passive approaches to cystitis management: on the one hand, people actively seeking medical confirmation; on the other, those who tend to minimize symptoms or forgo formal diagnosis.
Moreover, the data confirm what was anticipated: the lack of a standardized national clinical approach to diagnosing and managing cystitis. This absence translates into heterogeneous diagnostic practices and therapeutic decisions, both among patients and healthcare professionals.
Further evidence: about 10% report consulting a doctor without being prescribed any urine test. This points to a serious inconsistency in clinical practice: even when respondents interact with the healthcare system, diagnostic procedures are not applied systematically.
Pathogens identified among respondents who underwent testing
Subsequently, analysis focused on the subgroup of respondents who performed urine culture with antibiogram or laboratory urine testing, representing 70% of the total Italian sample.
Results mainly show the presence of Escherichia coli, found in about 55% of tested cystitis cases.
As expected, E. coli emerges as the predominant pathogen, in line with consolidated epidemiological evidence on urinary tract infections. The second most frequent response, however, was “no bacteria,”highlighting a heterogeneous subgroup of patients for whom urine culture showed no bacterial growth. This can be interpreted in different ways, falling into three main clinical situations: true abacterial cystitis, where urinary symptoms are present without a documented bacterial infection, often linked to irritative or inflammatory phenomena of another nature;
urine culture performed after antibiotic therapy, which can yield a false negative because bacterial load has already been reduced or eradicated;
incorrect urine collection, with contamination or inadequate sample storage compromising bacterial growth in culture.
Did you know?
Escherichia coli helps protect the intestine from harmful microbes and supports digestion by fermenting sugars to release energy. It also produces essential vitamins—B1, B2, B6, B12, K and others—important for skin, nerve, and metabolic health, acting at the same time as natural antioxidants that slow cellular aging.
Psychological implications of chronic and recurrent cystitis
This section focuses on one of the most significant and relevant aspects of the Dimann dataset: detailed information on the psychological impact of cystitis and the assessment of its effects on quality of life for those affected.
Among the various explored dimensions, the psychological and emotional burden of cystitis emerges as one of the most revealing and meaningful aspects of the Dimann dataset.
Cystitis often hides a deeper level of suffering that goes beyond physical discomfort: the recurrent nature of the infection, its unpredictability, and the limitations it imposes on daily life contribute to a constant sense of frustration and anxiety.
The relationship between stress and physical symptoms appears bidirectional:on the one hand, stress can increase susceptibility to infection and encourage recurrence; on the other, the discomfort and disruption of daily activities caused by cystitis tend to intensify tension and anxiety in everyday life. This self-reinforcing loop highlights the deep link between emotional wellbeing and physical health, showing how psychological strain can be both a consequence and a cause of the persistence of the condition.
In the dataset, self-reported experiences provide a direct perspective on how cystitis influences emotional wellbeing, self-perception, and social relationships.
Many respondents reported a decline in self-confidence, as well as a growing
sense of limitation in their ability to carry out normal daily activities—at work, in social or intimate settings, or during rest and leisure.
These constraints gradually erode a sense of autonomy and spontaneity, which are fundamental to a balanced life. These circumstances highlight the need to interpret cystitis not only as a transient infection, but as a condition capable of profoundly affecting psychological state and overall quality of life.
The emotional burden is both significant and underestimated, indicating the urgency of integrated care strategies that take into account not only the physical dimension, but also the mental and emotional dimension of the disease.
For these reasons, the information contained in the Dimann dataset regarding perception of cystitis, its influence on mood, daily life, and overall wellbeing represents a fundamental and long-awaited contribution to current research.. By documenting lived experiences of thousands of patients, the dataset captures dimensions of suffering rarely represented in traditional clinical research.
To explore this psychological and perceptual dimension, three key questions from the Dimann questionnaire were selected for analysis.
These items were chosen because, taken together, they offer a complete view of how people perceive cystitis and how it affects their emotional state and daily life.
- The first question asks respondents to define what cystitis represents for them, assessing how present the condition is in their lives—from a temporary nuisance to a constant and discouraging burden.
- The second question focuses on the concrete consequences of the infection, asking participants to indicate which aspects of their lives are affected by the need to urinate frequently.
- The third question explores the psychological sphere, allowing respondents to independently identify the emotional repercussions of cystitis—from loss of self-confidence to changes in habits and daily routines.
Taken together, these three perspectives provide a multifaceted understanding of how cystitis affects both the emotional and practical dimensions of people’s lives.
What is cystitis for you?*
An unexpected guest
An unwanted companion
A dead end
A nightmare
A hell
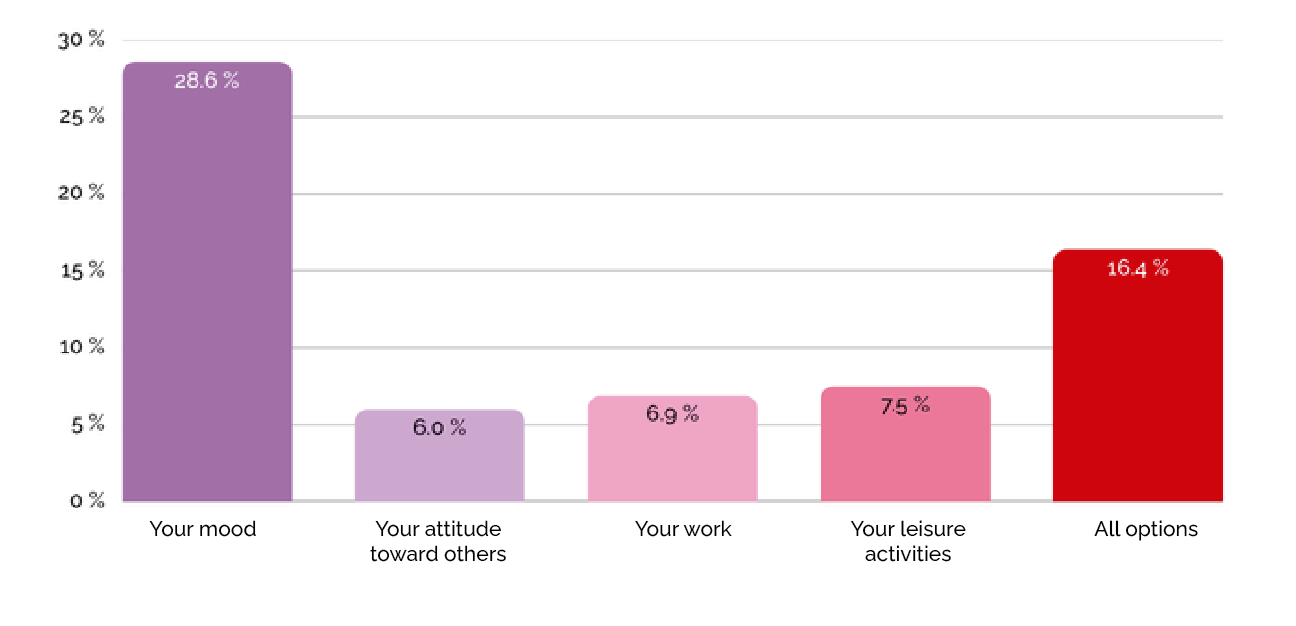
Going to pee many times a day affects…*
Your mood
Your attitude toward others
Your work
Your leisure activities
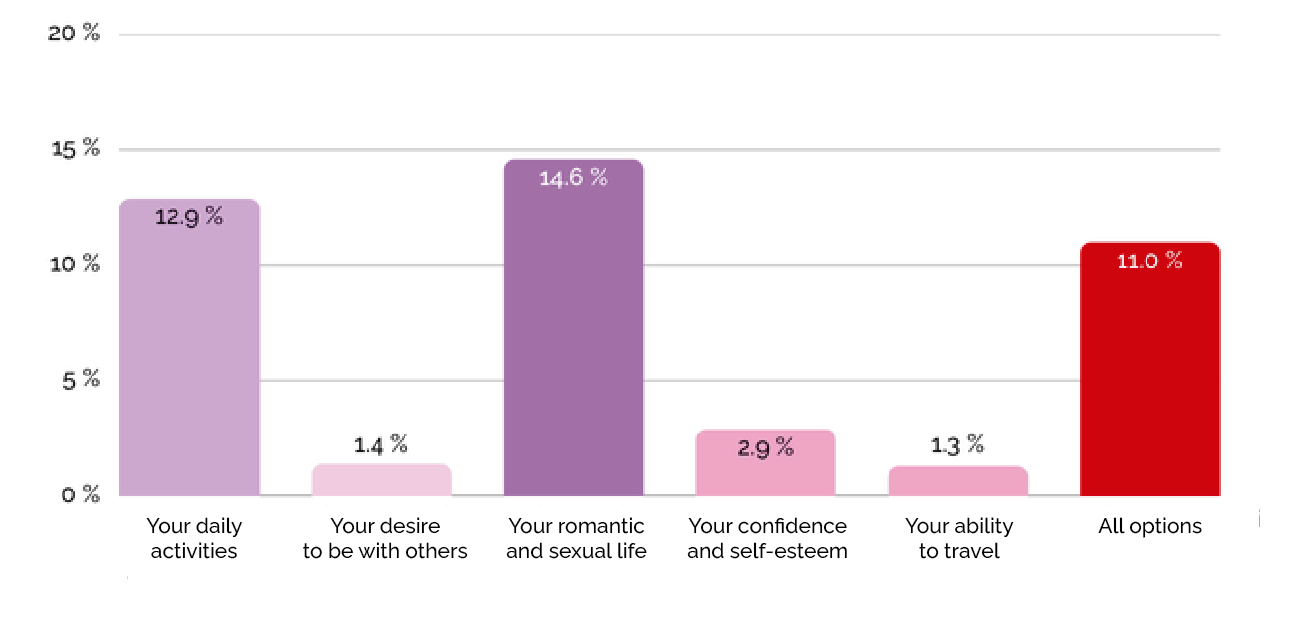
Having cystitis affects…*
Your daily activities
Your desire to be with others
Your romantic and sexual life
Your confidence and self-esteem
Your ability to travel
*More than one answer possible
What is cystitis for you?
The first question appears in the early stages of the questionnaire and invites respondents to describe how they perceive the infection.
It offers five possible responses,carefully worded to capture a wide range of emotional reactions and reflect different levels of psychological involvement with the condition. In addition, participants could select more than one optionto represent simultaneously the different facets of their emotional experience. This structure makes it possible to move beyond a single, uniform definition of cystitis, instead reflecting the complexity of how people internalize and experience their condition.
The resulting response distribution shows a spectrum of perceptions: for some, cystitis is an occasional and manageable nuisance; for others, it is a true “nightmare” that deeply affects daily life and emotional wellbeing.
As shown in Figure 7, respondents most frequently described cystitis as “a nightmare” (28%), an expression that reflects the profound emotional distress associated with recurrent or persistent symptoms.
The second most frequent description, “an unwanted companion” (19.1%), conveys the feeling of living with a constant, invasive presence—something tolerated, but never truly accepted.

Urinating many times a day affects...
When asked which aspects of their lives were most affected by the need to urinate frequently, respondents provided answers highlighting the strong impact of cystitis on daily habits and emotional wellbeing.
The most frequently selected option was “your mood” (28.6%),confirming how recurring symptoms and persistent discomfort directly affect emotional stability. The second most frequent response pattern was selecting all options (16.4%),as shown in Figure 8. This result underscores the multidimensional nature of cystitis’ impact, suggesting that many people perceive the condition as an all-encompassing burden capable of influencing every aspect of their lives. Moreover, mood emerged as the most consistently affected area: even among those indicating multiple compromised domains, mood was almost always included.
Having cystitis affects...
When identifying the areas of life most affected by cystitis, the most frequently selected response was “romantic and sexual life” (14.6%), confirming the profound impact of the condition on intimacy and emotional relationships (Figure 9).
Beyond this specific sphere, responses again show the pervasive nature of cystitis in everyday life: “daily activities” emerged as the second most frequent category, reflecting how recurrent symptoms and physical discomfort interfere with personal routines and perceived autonomy.
A considerable number of respondents, once again, selected all available categories.
Particularly significant, however, is the fact that over 15% of participants chose both “romantic and sexual life” and “daily activities,” highlighting a strong intersection between emotional and practical consequences of cystitis.
Conclusions
The purpose of this white paper was to present the analytical and exploratory potential of the Dimann dataset, collected over three years as part of a survey of D-mannose buyers, with the aim of identifying the most suitable product for each user profile.
The dataset represents a valuable and promising resource in the current landscape of cystitis research, an area where high-quality data remain limited and many relevant dimensions are often overlooked.
In particular, while the significant role of behavioral factors in the onset and recurrence of cystitis is recognized, these aspects have received little scientific attention over time. Furthermore, the dataset highlights the profound impact of cystitis on people’s lives—and especially on women, given the higher prevalence of the condition in females.
Previous studies show that cystitis can compromise daily life and psychological wellbeing, often generating a vicious cycle in which stress caused by the disease contributes to new recurrences. However, despite these significant implications, research on the psychosocial burden of cystitis remains underdeveloped, neglecting both the impact on affected individuals’ lives and its potential role in worsening the condition itself.
Even in this preliminary analysis of the described dynamics, data revealed that mood is the aspect most frequently influenced by cystitis, emerging as the most impacted both as a single choice and across the majority of combined responses. This observation strengthens evidence of cystitis’ strong psychological component and underscores the importance of considering emotional wellbeing both in research and in therapeutic approaches.
The impact on mental health and self-esteem becomes even more evident when comparing these results with responses about repercussions on daily life. In this sense, the areas most frequently indicated as affected were intimate/relational life and daily activities, often selected together.
Taken together, these results outline a deeply complex condition, highlighting the need for a more holistic approach that recognizes psychological and social repercussions as much as physiological manifestations.
Addressing cystitis therefore requires not only appropriate medical treatment, but also active and ongoing research on its impact on lifestyle and condition management strategies.
Such an approach is essential to fully grasp the complexity of the pathology and develop effective and sustainable therapeutic strategies—not only clinically and economically, but also in terms of patients’ long-term well-being.
Highlights
In Italy, truly comparable national data do not exist due to differences among regional surveillance systems and the absence of studies on risk factors specific to the Italian context. The Dimann dataset can help bridge this gap.
Cystitis has a strong psychological influence. Most patients describe the condition as a nightmare.
Diagnostic behaviors reveal systemic inconsistencies. About 70% of respondents underwent urine culture or lab testing, while 19% took no diagnostic action, highlighting heterogeneous medical practices and the need for awareness-raising.
E. coli remains the predominant pathogen, accounting for about 55% of identified infections.
Nearly 30% of respondents report that cystitis affects their intimate and sexual relationships. This sphere, like mood, is highly recurrent and appears alongside impaired daily activities in a further 15% of cases.
Stress is a known risk factor, yet it is also an overlooked consequence of the condition. 28% report that cystitis affects their mood, while over 10% state it impacts every aspect of their lives.
Mood is the most compromised aspect: it is not only the most frequent response, but it also appears in combination with almost all other impact areas, indicating emotional distress as a cross-cutting element of the cystitis experience.
Colophon and credits
Issued by:
The European Cystitis Observatory (ECO).
Conclusions and interpretations are those of ECO.
Prepared by:
Nami Consulting (Maria Ascolese, Erica Ravarelli) using a dataset provided by Dimann.
Funding:
Yellow People Lab (owner of the Dimann brand). (https://ypl.ventures/Ypl)
Clinical review:
Dr. Oreste Risi, MD (Urologist).
How to cite:
European Cystitis Observatory (ECO). (2026).
Understanding Recurrent and Chronic Cystitis –
Psychological impact of an ongoing battle.
Evidence from Italy. (Versione V1). Zenodo.
https://doi.org/10.5281/zenodo.18185934Doi 10 5281
© 2026 Yellow People Lab Srl. Creative Commons Attribution 4.0 International
References
- Foxman, B. (2003). Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Dis. Mon. , 49(2), 53–70.
- Boni, A. (2018, April 3). Cistite: MELIUS PREVENIRE. Medici Oggi, Milan.
- Scholes, D., Hooton, T. M., Roberts, P. L., Stapleton, A. E., Gupta, K., & Stamm, W. E. (2000). Risk factors for recurrent urinary tract infection in young women. J Infect Dis, vol. 82.
- Li, R., & Leslie, S. W. (2025). Cystitis [Updated 2023 May 30]. In StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482435/
Ncbi Books - Kurotschka, P. K., Gágyor, I., & Ebell, M. H. (2024). Acute Uncomplicated UTIs in Adults: Rapid Evidence Review. Am Fam Physician, 109(2), 167–174. PMID: 38393801.
- AOGOI. (n.d.). Le infezioni delle vie urinarie nelle donne dalla pre-adolescenza all’età adulta [Internet]. Roma: AOGOI. https://www.aogoi.it/media/7921/infezioni-vie-urinarie-donne-min.pdf
Aogoi Media - Zamparini, E., & Viale, P. (2012). Bacterial and fungal urinary tract infections: epidemiology, pathogenesis and clinical management. G Ital Nefrol., 29(S56), S3–S7.
- Naber, K. G., Tirán-Saucedo, J., Wagenlehner, F. M. E., & RECAP group. (2022). Psychosocial burden of recurrent uncomplicated urinary tract infections. GMS Infect Dis., 10, Doc01. https://doi.org/10.3205/id000078. PMID: 35463815; PMCID: PMC9006425.
- Paris, D., Caltagirone, M., Minzulli, P., Valzano, A., Ferrara, F. E. O., & Magliano, E. (2020). Epidemiology and antibiotic resistance in community-acquired lower urinary tract infections in the Milan area. Microbiologia Medica, 35(2).
- Fernandez, M. M., Bektas, M., Colosia, A., Kuper, K., Al-Taie, A., & Kotb, R. (2024). Evidence gaps in the burden of complicated urinary tract infection (cUTI). Poster presented at the 34th European Congress of Clinical Microbiology & Infectious Diseases (ECCMID), April 27, 2024, Barcelona, Spain.
- Causio, F. A., Golinelli, D., Diedenhofen, G., Silenzi, A., Ferro, D., & Baglivo, F. (2025). Fragmented but evolving: a response to the editorial “the Italian health data system is broken”. The Lancet Regional Health – Europe, 51. https://doi.org/10.1016/j.lanepe.2025.101256
- Ahn, St., & Oh, Mm. (2022). Importance to Promote Awareness in Patients with Recurrent Cystitis. Urogenit Tract Infect., 17(3), 71–75.
- Cai, T., Tamanini, I., Collini, L., Brugnolli, A., Migno, S., Mereu, L., Tateo, S., Pilatz, A., Rizzo, M., Liguori, G., Bonkat, G., Wagenlehner, F. M. E., & Bjerklund Johansen, T. E. (2022). Management of Recurrent Cystitis in Women: When Prompt Identification of Risk Factors Might Make a Difference. European Urology Focus, 8(5).
- European Association of Urology. (2025, September). Public survey on knowledge and experience of urinary tract infections [Survey commissioned for Urology Week, 22–26 September 2025]. Supported by GSK.

